Surgery
Microbiology of M.leprae
The aetiological agent of leprosy is Mycobacterium leprae. It is a strongly acid-fast rod-shaped organism with parallel sides and rounded ends. In size and shape it closely resembles the tubercle bacillus. It occurs in large numbers in the lesions of lepromatous leprosy, chiefly in masses within the lepra cells, often grouped together like bundles of cigars or arranged in a palisade. Chains are never seen. Most striking are the intracellular and extra-cellular masses, known as globi, which consist of dumps of bacilli in capsular material.
The laboratory diagnosis of Leprosy is made by:
. Histology
2. Examination of appropriate Ziehl-Neelsen-stained skin smears for AFB
Bacilli are found in polar Lepromatous leprosy (LL), Borderline (BB) and its variants Borderline Lepromatous (BL). They are scanty in Borderline tuberculoid (BT) and are not found in polar tuberculoid (TT).
Instructions for preparation of Shin Smears
These are best performed by experienced staff. The nodule of plaque Is cleaned with ether or any suitable disinfectant. The skin is gripped tightly between thumb and forefinger of the left hand to exsanguinate the lesion. An incision, 5 mm long and 3 mm deep, is made in the skin between the fingers of the left hand with a small bladed scalpel, the pressure on the fingers being maintained. The base of the wound is scraped several times in the same direction, so that tissue fluid and pulp collects on the blade and this is smeared \on a labeled glass slide. There should be minimal blood on the specimen. Smears from ear lobes are made in the same manner. The incision is made along the lateral edge of the pinna, the latter being compressed between thumb and forefinger. 6-8 smears are made from each patient. The sites are recorded and it is preferable to repeat smears from the same site when repeat specimens are taken later. Slides should be heat fixed if there is a delay in reading in the laboratory
Smears from Nasal Secretions
These smears are essential in deciding whether a patient is infectious. They are always positive in untreated (LL), some (BL) and negative in all cases of (BB), (BT), and (II). The patient is requested to blow into a tissue and smears are made with a scalpel onto glass slides (2-3).
Reporting conventions
The smears obtained are stained by the Ziehl-Neelsen method and are decolorized with I % acid alcohol.
Two indices which depend on observation of M. leprae in smear from skin or nasal smears are useful in assessing the amount of infection, the viability of organisms and also the progress of patient under treatment. They are the morphological index and bacteriological index.
Bacteriological Index (Bl)
The Bl as proposed by Ridley; is an index of the bacillary load in the patient. It is calculated by counting six to eight stained smears under the I OOx oil immersion lens. The mean index is calculated The results are expressed as a semi-logarithmic scale from I + to 6+ as given below.
Bl Interpretation
1+ I to 10 bacilli per 100 high power (oil immersion) fields
2+ I to 10 bacilli per 10 high power fields
3+ I to 10 bacilli per high power field
4+ 10 to 100 bacilli per high power field
5+ 100 to 1000 bacilli per high power field
6+ > 1000 bacilli per high power field
Reference may be made to the term 'globi' in some reports. These are clumps of bacilli and are generally found In LL. The dumps are derived from micro-colonies in macrophages.
In bacilliferous (MB) patients, on treatment, it may be found that there is no fall (or only a slight fall) in the Bl during the first 12 months, because dead and living bacilli are both being counted (both being stained by carbol fuchsin), but after this, a steady fall in density of bacilli takes place over the next 5-10 years. With adequate and effective treatment Bl declines by I log /year i.e. I + per year.
Morphological index (Ml):
A more sensitive index of bacteriological improvement is required for patients; hence the introduction of a system of classifying the bacilli in smears into two groups, solid stained (viable), and irregularly-stained (dead). Gerhard Hansen, in 1895, was the first to put forward the view that granular bacilli should be considered dead.
Ml interpretation
The Ml is an index of viability of the bacilli. Two hundred discrete bacilli are evaluated if possible. The Ml is equal to the percentage of viable bacilli. The Ml in untreated multi-bacillary leprosy usually ranges between 25 and 75 and should decline to 0 after 4 to 6 months of effective modem chemotherapy.
This index indicates whether the disease is active, responding to treatment, whether the patient has defaulted on treatment or developed bacterial resistance to chemotherapy. An increase in Ml therefore indicates a worsening of die patient's condition, and a decrease indicates improvement. Note that pauci-bacillary lesions may not be assessable for the Ml.
Reference:
Laboratory techniques of leprosy, 1987; WHO/CDS/LEP/86.4
WHO expert committee on leprosy. 7 report WHO Technical report series 1998/874
Leprosy - Still a Burning Problem
Dr. S. S. Chaudhary
Professor & H.O.D., Department of Dermatology, RIMS,Ranchl
Introduction
Leprosy (Hansen's disease / Hanseniasis) Is a chronic disease caused by Mycobacterium leprae, infectious in some, affecting the peripheral nervous system, the skin and certain other tissues.
Why Leprosy cannot be controlled or Eradicated?
1. ETIOPATHOLOGICAL FACTORS -
A. GENETIC FACTORS: (affect polymorphism)
Tuberculoid - HLA Dr2, HLA Dr3
Lepromatous - HLA Dq I, TNF a, IL-10, VITAMIN D receptors, Toll cell like receptors
B. ENVIRONMENTAL AND SOCIAL FACTORS
Overcrowding, Poor nutrition, Poverty, Ignorance, Social taboos €y prejudices
2. LEPRA REACTIONS
Acute episodic exacerbations & remissions of symptoms and signs of inflammation during active stage of leprosy and directly related to leprosy
TYPES - TYPE 1 & TYPE2
TYPE 1 REACTION -
Due to rapid change in CMI either for better or for worse; seen in BT, BB & BL It Is better called Upgrading or Reversal reaction; due to rapid increase in CMI as better response to treatment or in puerperium Irrespective of treatment
TYPE 2 RECTION -
Due to antigen-antibody reaction in presence of complement and not due to change in CMI.
It is an Immune Complex syndrome seen in LLp &LLs and rarely in BL
CONDITIONS CAUSING DOWNGRADING REACTIONS
Pregnancy, Malaria, Malnutrition, Contraceptive Pills
FACTORS PRECIPITATING TYPE 2 REACTION -
Intermittent infection, Injury, Surgical operation, Physical, mental stress, Protective immunizations, Strongly positive Mantoux test, Pregnancy & Parturition, Ingestion of Potassium Iodide, Antileprosy drugs
TREATMENT OF TYPE 1 REACTION
Basically treat neuritis - the major cause of morbidity
Rest to the part affected
Analgesics
If severe-then STEROIDS {anti-inflammatory dose} can be given.
Later, if tenderness & thickening of nerves persisting then Perineural infiltration with TRIAMCINOLONE
TREATMENT OF TYPE 2 RECTION
Bed rest advised as there are constitutional symptoms
Analgesics and Antipyretics
Systemic Steroids-especially in case of iritis (not responding to steroid eye drops), epididymo-orchitis or erythema necroticans
RECURRENT TYPE 2 REACTION
Systemic steroids starting at 40mg/day then tapering at 2 weeks interval Oral Thalidomide (in steroid dependent cases) at a dose of 300-400mg/day then tapering after the lesions subside.
3. DAMAGE OF THE PERIPHERAL NERVES -
The longer the delay between appearance of first symptoms of leprosy and the start of treatment, the more likely is the damage to nerves
Nerve damage will cause following physical problems -
1. Problems in eye due to motor and sensory loss
2. Motor and sensory loss in hand
3. Motor and sensory loss in foot Useful interventions for long term deformities-Home based self care
Simple intervention organized in local clinics and hospitals Referral services for more complex interventions
4. ADVERSE EFFECTS OF MDT
1. Minor problems : (i) Rifampicin - red urine, G.I.T upset, (il) Clofazimine -brownish discoloration dryness of skin, G.I.T upset, (iii) Dapsone - anaemia, G.l.T.upset
2. Major problems : (i) Rifampicin - jaundice, shock, purpura, renal failure, (il) Clofazimine - acute abdomen, (iii) Dapsone syndrome - itchy skin rash, fever, urticaria,
lymphadenopathy, (iv) Dapsone - SJS
5. COMPLICATIONS OF ADVANCED UNTREATED DISEASE
If patient is not diagnosed early and remain untreated for a very long period then patients come with unusual presentations -
Eye problems - Exposure keratitis, Superficial punctuate keratitis, Miliary lepromata, Insidious iritis, Sclerosing keratitis, Ciliary staphyloma, Iris pearls, Secondary cataract, Secondary glaucoma, Retinal nodule Facial and other deformities - leonine fades, facial palsy, hoarseness of voice, gynecomastia, osteomyelitis (bone absorption)
Internal medical conditions - bacilliary infiltrations of adrenals and renal can cause medical problems though very rare, these days
6. SHORTFALL IN GOVERNMENT CONTROL PROGRAMS
I. Untrained or improper trained health personnel - engaged in eradication and control programs
2. Defect in delivery system of drugs and other facilities provided by the government/ NGOs
7. Lack of pre-treatment and post- treatment counselling and lack of viewing "take home message" to each and every patients after completion of treatment
8. PSYCHOSOCIAL PROBLEMS:
The prevailing ignorance of the public regarding the facts of the disease
Deep rooted prejudices, fears and wrong beliefs
The ostracism of sufferers by the society
Disability and disfigurement caused by pursuing regular occupation by patients
Stigma attached to the disease drives the patients underground without opportunities for early diagnosis, treatment and complete cure
Fatalistic attitude of patients and philosophic acceptance of the condition resulting in lack of enthusiasm for seeking treatment and continuing with the same
The occurence of deformities and plantar ulcers during disease and in spite of the usual treatment, making them indifferent and unconcerned
It needs mental, physical, social, economical and medical rehabilitation.
It includes all measures aimed at reducing the impact of disability of an individual enabling him or her to achieve independence, social integration, a better quality of life and self actualization.
Leprosy is a unique disease in many respects.
Mycobacterium leprae, the causative organism of leprosy, M. leprae multiplies very slowly. This feature is responsible for the unusually long incubation period (2-20 years).
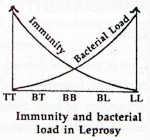
Importance of Host Immunity:
Most persons in a leprosy endemic area, like India, are exposed to the bacilli but do not develop the disease and have positive lepromin test. This is due to the immunity of the host.
The type of leprosy that a person develops is also dependant on host immunity. Persons with very poor or no immunity gradually develops into the lepromatous form and those with good immunity evolve into the tuberculoid form. Borderline varieties occur in those who have medium immunity. Many with very good immunity may have the indeterminate type or is not affected at all.
1) EPIDEMIOLOGY OF LEPROSY:
 Mode of Transmission:
Leprosy is usually transmitted by skin to skin
contact, but by droplet infection. Nasal droplets
of patients with lepromatous leprosy contain
thousands of bacilli, but have negative nasal
smears and are therefore mostly non- Infectious.
Mode of Transmission:
Leprosy is usually transmitted by skin to skin
contact, but by droplet infection. Nasal droplets
of patients with lepromatous leprosy contain
thousands of bacilli, but have negative nasal
smears and are therefore mostly non- Infectious.
Incubation period:
Usually 3-5 years. (Some cases recorded upto 20 years)
Classification of Leprosy
Ridley-Jopling classification. It is based on four parameters viz, dinical (morphology and distribution of skin lesions and nerve involvement), bacteriological (bacteriologic index on skin smears), histopathological (type of granuloma, tuberculoid or macrophage) and immunological (e.g. lepromin positivity).
2) INDETERMINATE:
Clinical
Few poorly defined, hypoplgmented, macules, ususlly smaller than 5 cm, with partial or no loss of sensation or sweating, usually over face or extremities of children are typical.
Bacteriology
Usually negative.
Histopathology
There is no granuloma; only sparse perivascular, periappendageal and peri and intraneural infiltrate of lymphocytes.
Immunology
Lepromin negative.
3) TUBERCULOID (TT):
Clinical
One or two, well defined, hypoplgmented or erythematous atrophic patches
or plaques, (commonly 3-5 cm in diameter), with a dry surface are noted over
extremities or face. Sensations are severely affected. Sweating is usually
absent. A cutaneous nerve or a nerve trunk in the vicinity may be enlarged.
Bacteriology
Negative.
Histopathology
Tuberculoid granuloma consisting of epitheloid cells and lymphocytes, with prominent Langhan's giant cells, close to the epidermis; no subepidermal free grenz zone. Granuloma is along a nerve (elongated).
Immunology
Lepromin test ++
4) BORDERLINE TUBERCULOID (BT):
Clinical
One or two large or many small hypopigmented or erythematous patches or plaques with a dry surface are present. Lesions are not as well defined as in TT leprosy. Satellite lesions are seen commonly beyond the margins of larger lesions and are a feature of BT leprosy. Distribution of lesions is asymmetrical. Sensations and sweating over the lesions are affected. One or two nerve trunks in the vicinity of the lesions are usually thickened.
Bacteriology
Usually negative; occasionally I +.
Histopathology
Tuberculoid granuloma consisting of epitheloid cells and lymphocytes with absent or small and less prominent Langhan's giant cells; granuloma rarely impinges on epidermis and is usually along a nerve (elongated).
Immunology
Lepromin test weak 4- or negative.
5) MID-BORDERLINE (BORDERLINE BORDERLINE, BB):
Clinical
Compared to BT patches and plaques increase in number but decrease in size. They lend to be more 'infiltrated'. Sensations and sweating are partially present, and lesions have a bilateral distribution involving extremities and trunk.
A morphology characteristically is 'inverted saucer' like 'infiltrated' annular plaque, sloping peripherally and merging gradually with the normal skin and a punched out center that is free of erythema or infiltration.
Bacteriology
Usually I + or 2+ occasionally 3+.
Histopcrthology
Loosely arranged granuloma of histiocytes, many of which resemble epitheloid cells, along with lymphocytes and a few foreign body giant cells characterize this form. Free subepidermal grenz zone is present Elongated granulomas along a nerve are still identifiable.
Immunology
Lepromin negative.
6) BORDERLINE LEPROMATOUS (BL):
Clinical
In BL, the plaques further increase in number but decrease in size, are poorly defined, have an oily surface. Sensations and sweating are partially or fully preserved and the lesions are not only bilateral but tend to become symmetrical. Few erythematous infiltrated nodules may be present, usually over face.
Bacteriology
Usually 2+ or 3+ occasionally 4+
Histopathology
Histiocytes and lymphocytes that tend to be clustered within the poorly defined and patchy granuloma with a distinct free subepidermal zone are seen in this form. Granulomas around nerves in deep dermis are rounded with a tendency to show onion peeling appearance. Foamy macrophages are seen later in the course of the disease.
Immunology
Lepromin negative.
7) LEPROMATOUS LEPROSY (LL):
Clinical
Numerous nodules or faintly hypopigmented macules or patches are characterize this type. Diffuse infiltration of the skin of the face and distal extremities is common. The lesions become ill defined, have oily surface, sensations and sweating over the lesions are usually preserved and lesions are bilaterally symmetrical.
Bacteriology
Usually 3+ or 4+, occasionally 5+ or 6+
Histopathology
Diffuse granuloma of monomorphic histiocytes and uniformly scattered lymphocytes involves the whole of dermis except the subepidermal free grenz zone. Foamy macrophages, some of which may be foamy giant cells, predominate over histiocytes during the later phase of the disease. Nerves in the deep dermis show an onion peel appearance.
Immunology
Lepromin negative.
8) COMPLICATIONS OF LEPROSY:
Leprous Infiltration:
Advanced LL type cases to loss of upper incisors, saddle nose and perforation of nasal septum or palate, Leonine fades, loss of lateral half of eyebrows etc. Diffuse hand or foot swelling may overlie leprous dactylitis.
Effects of Sensory Loss:
Symmetrical glove and stocking type anesthesia occurs in LL type. In other types of leprosy, only affceted regions are anesthetic. Long term effects of this sensory loss include gradual shortening of fingers and toes that results from repetitive subclinical trauma, traumatic ulcers and scars follow handling of tools, bums while cooking, smoking etc. Trophic ulcers over pressure bearing parts of die foot is an extremely common cause of disability in leprosy. They result from the repetitive subclinical trauma of walking, running, jumping encountered by a dry fissured foot that lacks pain sen-sation. Heads of first and fifth metatarsal and heel are the commonest sites of breakdown.
Effects of Autonomic Nervous System Affection:
Loss of sweating leads to dryness of feet, fissuring of soles and ichthyosis of extensor aspects of extremities. Loss of vascular tone leads to edema feet.
Effects of Motor Damage:
Function of muscles is compromised early, much before deformity sets in. Ulnar and median nerve palsy affect hand function. Ulnar nerve palsy at the elbow leads to ulnar claw flexion of interphalangeal joints involving the 4th and 5th fingers and flattening of hypothenar eminence. Median nerve palsy at the wrist leads to median daw or ape thumb deformity. Radial nerve palsy results in wristdrop.
Foot drop occurs due to lateral popliteal affection at the knee whereas hammer toes are the result of posterior tibial palsy at the ankle. Facial palsy occurs due to involvement of facial nerve at its point of emergence from the skull. Other motor nerves are uncommonly involved.
9) DIAGNOSIS OF LEPROSY:
Demonstration of M. leprae in the skin is not always possible in many cases of tuberculoid, borderline tuberculoid and indeterminate leprosy. These patients constitute the majority of leprosy cases and hence, a correlation of clinical features with findings of skin biopsy and sweat test are essential to reach a diagnosis of leprosy in them.
Cardinal Signs of Leprosy:
Ordinarily most patients with leprosy can be diagnosed as such if at least one and preferably two of the following cardinal signs are present. They include:
1) Loss or diminished sensation over a skin lesion (patch or plaque).
2) Presence of add fast bacilli in skin lesions.
Thickened peripheral nerves, especially in leprosy endemic regions.
10) INVESTIGATIONS IN LEPROSV:
Shin smears:
Smears are taken from both ear lobes, forehead, chin and a skin lesion. This is done by the silt and scrape method and stained with Ziehl Nielson stain. They provide a rapid method for diagnosis, classification and monitoring of therapy.
Bacteriological index signifies the density of bacilli in smears and is indicated as 0, I +, 2+, 3+, 4+, 5+ and 6+. As a broad guideline, index of 0 corresponds with TT and some BT cases, I + to 2+ with some BT and BB cases, 2+ to 3+ with some BB and BL cases and 3+ to 6+ with LL cases.
Morphological index ( MI) shows the number of live bacilli in smears. M. leprae may stain as solid rods, fragmented rods or granules. Solid rods are considered live bacilli. Ml gives a better indication of infectivity of a case. It falls rapidly to zero within 4-8 weeks of starting therapy in muttibadllary cases.
Shin biopsy:
In tuberculoid leprosy, there is a well defined tuberculoid granuloma, consisting predominantly of epitheloid cells and lymphocytes, that impinges on the epidermis. Granuloma commonly Involves and destroys cutaneous nerves.
In lepromatous leprosy, a diffuse granuloma of foamy macrophages involves the entire reticular dermis but spares the papillary dermis. Stains for acid fast organisms reveal them to be present intracellularly within macrophages. An intermediate picture is seen in borderline varieties of leprosy.
Sweat Test:
It compares the amount of sweating from affected site with that from a corresponding unaffected site on opposite side. Test sites are injected with 0.2 ml of 1:1000 pilocarpine nitrate, painted with iodine and powdered with starch. Starch powder turns blue in the presence of sweat. A rapid method is to use bromophenol blue impregnated paper for comparison of amount of sweat. The dye turns blue on contact with sweat. This is an important clinical test that differentiates macules of leprosy from other macules.
Nerve biopsy
It is useful for patients in whom only nerves are affected. Only the purely sensory nerves can be biopsied.
Nasal smears
Demonstrate M. leprae in LL.
Histamine test
Injection of histamine fails to cause flare in leprosy macules as compared to macules due to other causes.
Lepromin Test
Intradermal Injection of lepromin evokes a granulomatous response In the skin. Positive test indicates infection (not necessarily disease) and good immunity to it, i.e. either a disease free normal person orTT/BT leprosy.
11) MANAGEMENT OF LEPROSY
Dapsone mono-therapy which was used earlier is completely outmoded and has been replaced by a multidrug therapy (MDT) consisting of two or three drugs for paudbadllary and mukibaciliary leprosy respectively. This has changed the scenario of Leprosy.
Fixed Duration MDT for Paucibacillary (smear negative) Leprosy:
Includes:
i) self-administered Dapsone 100 mg daily (at bedtime) and
ii) supervised administration of Rifampicin 600 mg (preferably before food) once a month (called a pulse) for 6 months.
Fixed Duration MDT for Multibacillary (smear positive) Leprosy:
Includes:
i) self-administered Dapsone 100 mg daily,
ll) self administered Clofazimine 50 mg dally (after food),
iii) supervised administration of Rifampicin 600 mg and Clofazimine 300 mg once a month (called a pulse). Therapy is to be continued for a fixed period of two years in spite of the results of skin smears. The twenty-four pulses are to be completed during a maximum 36 months.
The dosages given above are for adults. Proportionately lower dosages are used for children. It is extremely important to patient compliance during thecomplete course.
There may not be any visible change In the skin lesions in patients with macules and patches during or even at the end-of therapy. Lost sensations and musde function may or may not be regained in part or full.
Clinical Implication: This has to be explained to the patient before or at least during the early part of therapy. Otherwise there is risk of patient either losing faith in the therapy or, on the contrary, continuing therapy indefinitely, without informing the doctor.
Newer drugs in Leprosy :
Newer antileprosy drugs is expected in near future. Newer regimens may contain rifampidn, ofloxacin, minocycline and clarithromycin. The treatment duration may be reduced to as little as one month for murtibacillary leprosy and one day for paucibadllary leprosy.
Unfortunately, resolution of lesions is not hastened with these crash courses of antibiotics.
New WHO recommendations include single dose of 600 mg rifampidn + 400 mg ofloxadn + 100 mg minocycline for patients with a single lesion of leprosy.
WHO recommendation for treatment duration of MB leprosy is also shortened to one year now.
12) SOCIAL ASPECTS
Social Importance of Leprosy:
A problem with leprosy is the sodal stigma. It arises from deformities secondary to nerve damage due to leprosy. It started at a time when there were no medidnes and the mechanisms for developing the deformities were ill-understood. Today the deformities due to leprosy can be prevented and corrected to a large extent and effective drugs render a patient virtually non-infectious in 24 hours. The social stigma has reduced but still persist.
13) LEPRA REACTIONS:
Exacerbations of the disease process in leprosy are termed as reactions. They represent hypersensitivity reactions. Traditionally, reactions are classified into two types.
Diagnosis of lepra reactions:
As majority of lepra reactions occur during antileprosy therapy it is vital to identify the early warning signs of reactions.
The warning signs are pain and tenderness of skin lesions and crops of new painful skin lesions with fever and arthralgia. It is frequently possible to reverse the damage partially or completely by instituting prompt therapy.
TREATMENT OF LEPRA REACTIONS:
Type I - Downgrading type I reactions are usually mild and are due to lack of therapy which allows a patient to downgrade along the leprosy spectrum (e.g.fromBTtoBL).
Upgrading type I reactions are commoner and severer than downgrading types and occur during the first 6 months of initiating antileprosy treatment.
Type II - Lepra reactions respond dramatically to systemic steroids. Dosage and tapering schedule of steroids is similar to type I reactions. However, relapses are frequent with steroid reduction. Oral NSAIDS, clofazimine (200-300 mg per day for many weeks), chloroqulne, colchicine (0.5 mg tds) and zinc (220 mg OD), supplement steroid action and allow their smoother taper. In unresponsive or relapsing reactions thalidomide 100 mg 3-4 times a day is the drug of choice. It is absolutely contraindicated in women of child bearing age group. Iritis, orchitis, glomerulonephritis need to be appropriately attended to.
Summary:
Type I reaction - Sudden edema and erythema of existing lesions of leprosy with or without pain indicate Type I reaction. Neuritis of the nerve trunk in the vicinity is commonType I reaction signifies change in immune status for better (within 6 months of initiating therapy) or for worse (lack of treatment). Neuritis is an indication for systemic steroid treatment which avoids nerve damage.
Type II reaction - Reaction tends to begin 6 months after initiating therapy for eprosy and is due to immune complex deposition. Crops of symmetrical, tender, bright red nodules and plaques occur over face and extremities (erythema nodosum leprosum). Lesions are transient lasting 2-10 days but new crops appear with severe constitutional disturbance. Neuritis may lead to nerve palsies. Iritis, orchitis, periostitis, myositis are common. High dose systemic steroids, instituted promptly and tapered gradually, avoid damage to nerves and organs.
14) Prevention of Disability due to Leprosy
While deformity implies structural abnormality of a limb or face, disability includes even functional impairment like loss of sensations. Deformities in leprosy commonly result from either
a) Affection of Motor Nerves ( e.g. ulnar / median palsy leads to ulnar/ median claw, lat. popliteal palsy results in foot drop).
b) Affection of Sensory Nerves results into trauma and subsequent trophic ulcers.
Steps in disability prevention include:
a) Identify patients at risk - Patients in reactions or those who are likely to develop reactions, those with existing disability or those with enlarged nerve trunks even in absence of overt signs of neuritis.
b) Give preventive advice while supervising and ensuring regular therapy.
c) Be alert to early warning signs of leprous neuritis e.g. pain, tingiling along a nerve, worsening of sensation or muscle power.
d) Treat neuritis promptly with systemic steroids ( prednisolone) 40 - 80 mg /day for many weeks ) while antileprosy therapy is continued.
e) Physical therapy during neuritis: Rest and passive splints initially; passive exercises,active exercises and dynamic splints, later.
Correction of Deformities due to leprosy:
For the purpose of management, mobile deformities due to leprosy can be divided into early deformities, mobile deformities and fixed deformities.
Early deformities are usually associated with active neuritis and treatment is that of neuritis (i.e. prednisolone 40 - 80 mg / day tapered over many weeks). Rest, passive and active exercise and suitable splints are crucial in restoring power and reverting an early deformity.
Mobile deformities due to motor imbalance ( e.g. a claw hand ) can be corrected by a tendon transplant surgery which redirects functional tendons so as to restore cosmetic looks and function to a hand or a foot. Short duration, mobile deformities in young persons are ideally suited for surgical correction. Extensor carpi radialis longus or brevis tendon for correcting ulnar claw and flexor superficialis tendon of ring finger for correcting thumb deformity are two of the common operations in vogue.
Physical therapy for preparation of and follow up after surgery is important. Presurgical massage, wax baths improve deformity angles by softening the soft tissue contractures and improving blood supply. Presurgical muscle retraining prepares a patient for effective usage of the redirected muscle after surgery thereby improving the final result.
Fixed deformities can only be helped by oil massage, passive and active exercise, taking care that the insensitive limbs are not damaged. Provision of moulding hand grips for articles of day to day use reduces chances of trophic ulcers and improves function.